Overview of Arthritis
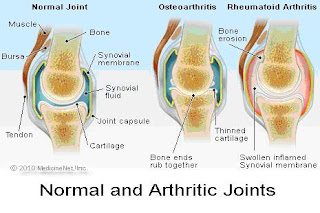
Arthritis is a chronic and debilitating condition which is caused by inflammation of the joints in the body. The inflammation within the joints results in pain, swelling and limited range of motion. There are over 100 different forms of arthritis, with the two most common forms being Osteoarthritis (OA) and Rheumatoid Arthritis (RA).
Often, people who suffer from arthritis tend to be inactive due to pain and fear of worsening their condition. Inactivity accelerates the disease progression, as well as increasing their chances of developing other conditions associated with inactivity such as obesity, heart disease, diabetes, hypertension, cholesterol to name a few.
Arthritis is the leading cause of disability in people over the age of 55 years and although there is no official cure to date, there are many ways of managing and controlling the condition to slow progression and manage pain.
Most Common forms of Arthritis
Osteoarthritis( ‘Wear and Tear Arthritis)
Osteoarthritis is also known as Degenerative Joint Disease, and is the most prevalent form of arthritis. It occurs due to the degeneration and loss of cartilage within the joints, which results in bone rubbing against bone. This friction leads to the formation of bony spurs and subchondral cysts, which causes joint pain.
Osteoarthritis is associated with normal wear and tear of the joints as a result of aging; however this process can be exacerbated by excess weight which places unnecessary pressure on the joints, heredity, or injury.
Commonly affected joints include the hips, hands, spine and knees.
Treatment Options
Rheumatoid Arthritis
This is a debilitating autoimmune( the body’s immune system mistakes some part of the body as harmful and attacks its own cells causing inflammation and destruction of the affected joints) disease which is characterized by inflammation and swelling of the synovial membrane which surrounds the joint , and the formation of pannus tissue within the joint. This eventually results in deterioration of the bone and cartilage, which results in pain, swelling, deformity and loss of movement within the joint. RA can be diagnosed by blood tests showing higher than normal levels of antibody rheumatoid factor (RF). RA Can be effectively controlled by the correct combination of medications, exercise, joint protection techniques and other self-management techniques.
Commonly affected joints are the wrists, hands, knees, feet and cervical spine. Symptoms of RA include morning stiffness lasting more than 30 minutes, acute flare ups and chronic inflammation as well as chronic pain and loss of joint integrity. RA usually fluctuates between bouts of acute flare ups (red, hot and swollen joints) and chronic inflammation.
Exercise Considerations
Clearance from a medical practitioner needs to be given before starting an exercise programme, especially in the case of RA, because rheumatic disease can have an effect on cardiovascular and pulmonary function. Exercise is also contra-indicated in the case of an acute flare up (especially in RA sufferers). It is also important to consider that deconditioned and poorly supported joints are at a high injury risk from high intensity exercise and unsupervised movement.
Benefits of Exercise
Moderate exercise improves cardiovascular fitness, neuromuscular fitness, flexibility as well as general health status. Arthritis-specific benefits of exercise include: improvements in muscle and bone strength, flexibility and endurance. This translates to improved range of motion and function in the joints, decreased joint swelling and pain, as well as decreased depression and anxiety. The correct types of exercise also improve the quality of the remaining cartilage in the case of OA, which slows the progression of the condition.
Goals of Exercise
- Joint protection
- Restoration and Maintenance of joint function
- Control the destructive inflammatory process
Beneficial Types of Exercise
In order to optimally improve the joint integrity, the following exercises are recommended:
- Low-impact aerobic activities(stationary cycling, swimming etc)
- Strengthening to improve muscle mass, which increases joint protection
- Avoid contact sports and sports involving rapid change of direction or prolonged one-legged stance position if there is either hip or knee involvement.
- Flexibility exercises to maintain and improve joint range of motion.
- Avoid overstretching and hypermobility, the goal is to achieve and maintain joints’ optimal range of motion.
- If there is pain and swelling following exercise, then the intensity or type of exercises should be changed to reduce load on the joint. An alternative mode of exercise such as swimming or cycling should be started or alternatively the intensity and duration can be adjusted.
- Stretching and light activity should be performed daily if possible, with moderate exercise being done 3-5 days per week.
- Avoid exercises that increase joint pain.
Other recommendations:
· Get plenty of sleep. Sleeping 8 to 10 hours a night and taking naps during the day can help you recover from a flare-up more quickly and may even help prevent flare ups.
· Avoid staying in one position for too long.
· Avoid positions or movements that place extra stress on your sore joints.
· Eat a healthy diet full of fruits and vegetables, which contain important vitamins and minerals, especially vitamin E.
· Eat foods rich in omega-3 fatty acids, such as cold water fish (salmon, mackerel, and herring), flaxseed, rapeseed (canola) oil, soybeans, soybean oil, pumpkin seeds, and walnuts.
· Apply capsaicin cream over your painful joints. You may feel improvement after applying the cream for 3-7 days.
· Lose weight, if you are overweight. This will decrease the unnecessary load placed on already compromised joints.